Kegel Health
Kegel strength is important for women and men of any age, but especially for women during and after pregnancy, and as a woman ages or approach menopause. Kegel exercises and kegel products can help with some forms of incontinence. Performing Kegel Exercises (aka Pelvic Floor Exercises) helps strengthen the kegel muscles that are used to stop the flow of urine. Doing these exercises regularly may improve incontinence.
Types of Kegel Devices
MedAmour carries many useful products and some of the best kegel balls specifically designed to help a woman strengthen her pelvic floor muscles. Kegel exercisers in this category include a range of options.
- Weighted kegel balls
- Kegel bars
- Vibrating kegel balls
- Vibrating or stimulating kegel devices
- App-controlled kegel devices with or without vibration
Weighted kegel balls
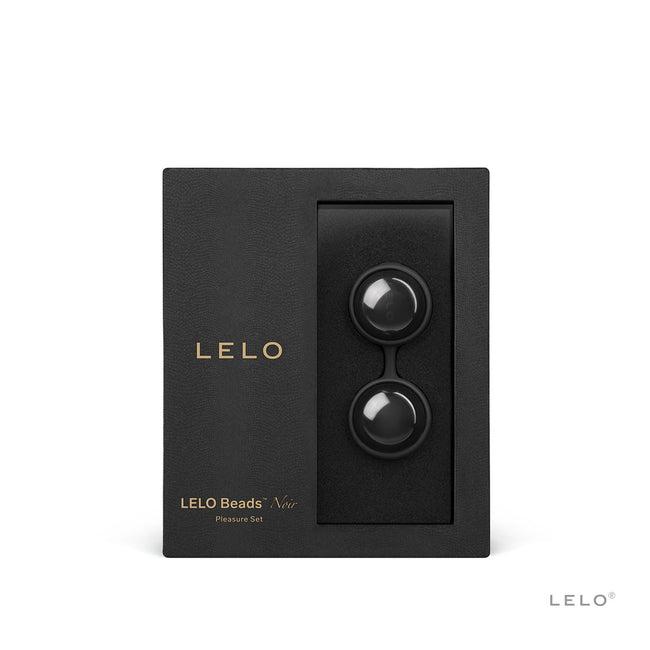
Weighted at varying levels (from light to heavier) and sometimes varying size (from large to small) to gradually increase strength in pelvic floor muscles, these devices are usually non-vibrating. Pelvic floor muscles strengthen by wearing the kegel exercise balls for a period of time and allowing the pelvic floor muscles to contract to hold them in place. Then can also be worn while performing kegel exercises. Examples include LELO Luna Kegel Beads and Je Joue Ami Kegel Balls.
Kegel bars
A weighted bar with a handle that allows the pelvic floor muscles to grasp the device, they are usually shaped with a bulbous end such as the Natural Contours Energie.
Vibrating kegel balls
Sometimes used for stimulation and pleasure, these types of kegel exercise balls vibrate to help a woman identify where her pelvic floor muscles are. Some vibrate in response to a kegel muscle contraction. Examples include G Balls 2 Kegel Balls and the Lovelife Krush Kegel Exerciser.
Vibrating or stimulating kegel devices
These devices are often designed to assist in strengthening pelvic floor muscles to alleviate incontinence. They may insert slim like a dilator and then expand and vibrate with pelvic floor contraction or vibrate to stimulate the pelvic floor muscles like the Apex Pelvic Floor Strengthener.
App-controlled kegel devices with or without vibration
Controlled by a smartphone app, these devices may either be kegel balls or shaped like a kegel egg. They connect by Bluetooth and use biofeedback to provide games to guide the user through their kegel exercises. A user can often track their progress, receive notifications (a huge help in remembering to do kegel exercises regularly!) and receive encouragement or rewards. These devices may or may not vibrate and can be used solely for pelvic floor exercises or also for pleasure. Examples include the Elvie (no vibration) and the kGoal (with vibration).
- 1 of 1