Pregnancy & Motherhood
Pregnancy, Motherhood & Sex
Both women and men have concerns about whether it is safe to continue having sex during pregnancy. For many years, it was believed that sex during early pregnancy could cause a miscarriage, and that sex during the last couple of months of pregnancy could cause infection or premature labor. There is no medical evidence or proof to support either of these beliefs during a normal, healthy pregnancy. Intercourse can safely continue until approximately the last month before delivery.
There are also couples who will abstain from sex during pregnancy for fear it might harm the baby in some way. Typically, a baby is well cushioned in a sac of amniotic fluid within the uterus and is, therefore, quite unlikely to be hurt by lovemaking.
It is important for pregnant women, and their partners, to discuss their needs, concerns, and desires openly and honestly. For instance, a woman may not feel like having sex during pregnancy, or her sexual needs may decline through her pregnancy. Simultaneously, she may find she has an increased need for other kinds of physical intimacy like cuddling, holding, or hugging. A pregnant woman might also experience a heightened sense of her body and become more sexually expressive—it just depends on the woman and that particular pregnancy.
A pregnant woman’s changing body size may make familiar lovemaking positions uncomfortable or even impossible. A couple can look upon this as an opportunity to be creative with sex by trying different positions, mutual hand stimulation or even oral sex (oral sex can be performed with caution: blowing air into the vagina during pregnancy should be avoided as it may lead to complications).
When to Avoid Sex During Pregnancy
Though it is rare, there are some instances when a doctor may advise against a woman having sex during pregnancy, such as when:
- There is a history of premature birth or labor
- Her water has broken
- She is bleeding
- She has placenta previa, a condition in which part of the placenta covers the cervix
- Either partner has a sexually transmitted infection
Sex After Delivery
A woman may be physically able to resume having sex as soon as 6 weeks after delivery, even if she has had a small tear to the perineum (the muscular tissue of the pelvic floor located between the vagina and the anus). Most women will wait at least 4 to 6 weeks, or until they get the OK from their doctor. Of course, this will depend on the type of delivery, how difficult it was, how many stitches were needed, if there were any complications, or if an episiotomy was performed.
A woman will experience some pain after delivery if she has a suffered a tear, or if an episiotomy was performed during delivery. To help ease the pain from the stitches, it is advisable to do the following;
- Place a cooled gel pad, or ice pack wrapped in a towel, onto the stitches for no more than 15 minutes every one to two hours. The ice will numb the area and prevent, or reduce, swelling.
- Expose stitches to the air for approximately 10 minutes, once or twice per day.
- Exercise the pelvic floor area by walking as much as possible. Doing Kegel exercises with your health care provider’s permission will also stimulate blood circulation to the area and facilitate the healing process.
- Take pain medicine only as prescribed by the doctor.
- If the pain worsens, or nothing seems to relieve it, there may be an infection present, and the stitches will need to be checked by a healthcare provider to ensure they are healing properly.
Emotional Readiness
There is a difference between when a woman is physically able to have sex after delivery, and when she feels emotionally ready to have sex. During the postpartum period, a woman’s body, hormones, lifestyle, sense of self, and relationships are in a state of change and flux. Lack of sleep, the constant demands of a newborn, her changing body image, and any anxieties about motherhood can have a negative impact on her sexual desire. Her partner may also be experiencing many of the same feelings.
The decision to resume physical intimacy is a very personal one. Some couples get back to their previous level of sexual activity with few problems, but for many couples, this requires some time, adjustment and communication. Even if sex is the last thing on a couple’s minds, it is important for the partners to find non-sexual ways to nurture and strengthen their bond. This will go a long way in reinforcing their relationship as a couple, and not just as parents.
Staying Connected
A couple should take some time each day to reconnect by talking, cuddling or sharing an activity they both enjoy. Accepting offers from trusted friends and family to baby-sit provides an opportunity for the couple to go out on a few, much-needed “dates.”
In addition to the new joys and responsibilities of parenthood, resuming intimacy is an important part of a relationship. Women, and their partners, often have questions about resuming sexual activity after having a baby as well as how to prevent another pregnancy.
When a couple decides to become sexual once again, it is important for them to communicate their feelings and expectations. The first time may be a little uncomfortable for a woman. Her vagina has recently been through some stretching and trauma, so it is important to take it slowly.
Setting the mood with candles and music, taking a relaxing bath, or giving each other massages can be effective ways to reduce anxiety and build desire. Remember, lovemaking does not have to start off with vaginal intercourse. A couple can gradually work up to that with plenty of foreplay that will ensure arousal. Even if lubrication was never a problem before, it is always advisable to utilize lubricant. This is especially true if the woman is breastfeeding, since that can make the vaginal skin thinner and drier (vaginal atrophy) due to decreased estrogen levels.
Most importantly, a couple needs to be patient. At first, sex may not feel the same since the woman’s body is still adapting to the physical changes that have taken place. With time and practice, a couple can regain their sexual chemistry.
Products that can help
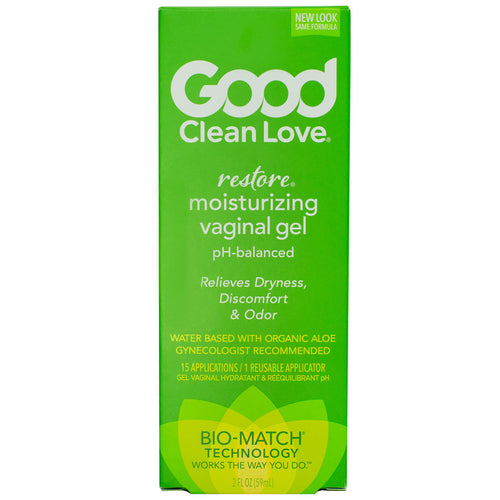
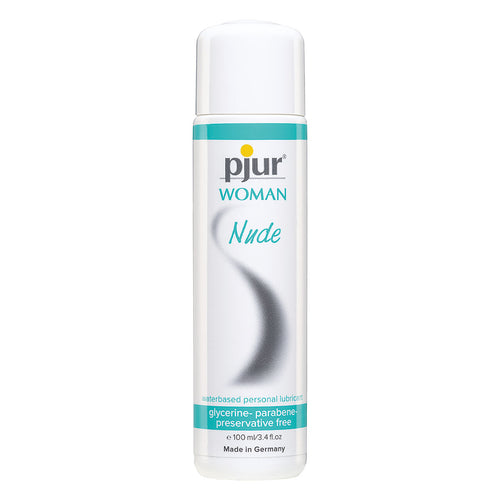
As mentioned above, a woman’s libido and lubrication can be affected during and after pregnancy. She may experience Vaginal Atrophy or even Anorgasmia for a period of time. Some products that help during this period and after include:
Lubricant
Fluctuations in hormones can affect a woman’s natural ability to lubricate. This is not necessarily an indication that she isn’t willing or that anything is “broken.” A lubricant, applied internally or externally can help soften the tissues and reduce friction. Be sure to select one that is gentle on your system. We recommend an all-natural or organic lubricant that is water or aloe-based.
External or clitoral vibrator
Stimulation to the clitoris with a vibrator or oral stimulation can increase arousal, potentially increasing lubrication. This will allow a woman to experience pleasure without penetration that might still be painful.
Massage oils and games
Relaxing, setting the mood, and being sensual can be a big part of enjoying sex after having a baby. Although it may be hard to set aside time with a newborn in the other room, a couple can make time for a romantic game or use massage oil to reconnect with each other’s bodies.
Nursing
A woman’s breasts are designed for pleasure, and nourishing an infant. A woman, and/or her partner may have mixed feelings about whether her breasts should belong exclusively to the baby while she is still breastfeeding. While there is no right or wrong answer, if a woman’s nipples are cracked and sore, it is best to leave them alone.
It is important to note that lactating women can leak milk from their breasts due to direct nipple stimulation, or from orgasm even if the breasts are not touched. The amount varies from woman to woman from a few drops to a “squirt.” If this bothers either partner, breast stimulation should be avoided, and a bra, with an absorbent pad inside, should be worn. Nursing the baby prior to intercourse can help empty the breasts and make the woman more comfortable. In any case, a couple might want to keep a cloth, and a sense of humor, nearby.
If a woman is not going to be breastfeeding, it is important that nipple stimulation be avoided. That is because, after pregnancy, any nipple stimulation can initially cause hormonal changes that will continue milk production. During this time, the breasts may become sore and engorged. It is helpful for a woman to wear a well-fitting, supportive bra at all times until lactation stops. If the discomfort seems intolerable, taking Ibuprofen or Tylenol, and applying cool compresses, can be helpful. Vibration can be used to help stimulate milk production for pumping or to help loosen milk ducts.
Postpartum Depression
Although reduced sexual desire is very common after pregnancy and delivery, it can also be a sign of postpartum depression. Many women experience some moodiness, sadness, or anxiety in the period following delivery (the so-called “baby blues”), but this normally improves within a couple of weeks.
If a woman is experiencing prolonged or very intense sadness, or if she has any thoughts of harming herself or the baby, she needs to get immediate help from her healthcare provider, a counselor, or a crisis center.
Returning to a Non-Pregnant State
After delivery, a woman’s body will gradually, over time, revert back to its non-pregnant state as follows:
- During the first six weeks post partum, the uterus will gradually decrease in size.
- The loose skin and muscles of the abdomen will gradually tighten to some degree.
- There will be a small amount of bloody vaginal discharge, called lochia, for 4 to 6 weeks.
- A vaginal tear or episiotomy will usually be healed within 4-6 weeks, but the tissue continues to change and remodel for up to a year.
- A cesarean (“C-section”) scar will take about 6 weeks to heal completely. Until then, heavy lifting must be avoided.
How quickly the menstrual cycle resumes depends on whether a woman is nursing or not. If she is breastfeeding exclusively day and night, it can take a year or longer before it returns. If a woman starts supplementing with formula, or the baby begins to sleep through the night, a woman’s menstrual cycle will tend to return sooner, typically within 3-8 months. Non-nursing women tend to start menstruating as early as one month postpartum.
Fertility and Birth Control
A woman’s body will release its first postpartum egg before she begins menstruating again. If she doesn’t start using birth control or condoms as soon as she begins having sex again, she could get pregnant. Also, it is a myth that women who are breastfeeding are not fertile. There are many nursing mothers who have been surprised by an unplanned pregnancy.
Kegel Strength
Pregnancy and a vaginal birth can have a huge impact on a woman’s pelvic floor muscles. These muscles support the uterus and are used when pushing to give birth. In extreme cases, a woman may also experience pelvic organ prolapse. A new mother may experience “leaking” or urinary incontinence when laughing, sneezing, coughing, or during high-impact exercise like running. This may come as a total surprise since pre-pregnancy it was never an issue. It is important at this stage to regularly do pelvic floor exercises to tone and strengthen these muscles. These can be performed with various kegel exercise devices. Kegel exercise devices come in several types:
- Non-vibrating, non-powered, weighted balls
- Vibrating, weighted balls
- Vibrating balls or eggs
- App-controlled vibrating and non-vibrating balls or eggs. This style uses an app that includes “games” to encourage exercise and daily tracking similar to a wearable fitness tracker.
Motherhood
One of the biggest challenges as a mother is setting aside the time for herself to relax, rest, and experience pleasure. Some women may feel this is being “selfish,” however maintaining a sense of self and your body’s needs is important to remain present and well-balanced for your child. Even if a mother can’t make as much time as possible with her partner, she can also engage in masturbation and time alone in order to remind herself that she is still a sexual being. We hope that some of the books and products we provide here at MedAmour help women on their path to a new stage in life!
Related Women's Health and Wellness Resources:
Kegel Products: Which One is Right for You?